Chronic non-healing wounds are those which do not proceed through the normal phases of wound healing in an orderly and timely manner. There are several reasons why wounds can fail to heal as expected and, consequently, appropriate management requires an understanding of these causes.
The phases of wound healing
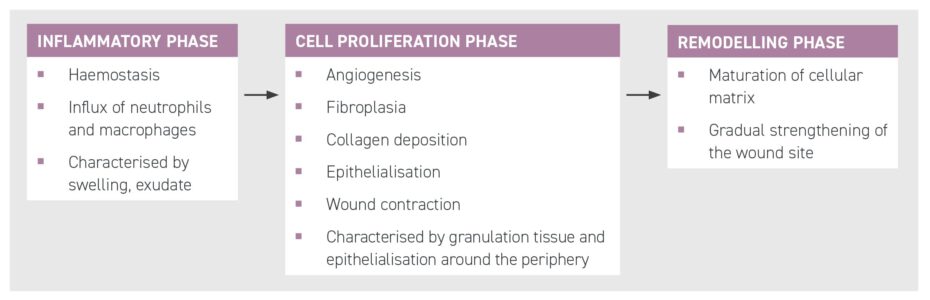
The phases of wound healing are shown in Figure 1. While we expect a wound to progress sequentially through these phases, some wounds, or even parts of the same wound, can be stuck in one phase. Usually this is the inflammatory phase and is caused by an ongoing source of inflammation, such as a sequestrum, movement, the presence of devitalised tissue, etc. The protracted presence of neutrophils and macrophages leads to an imbalance of mediators, resulting in fibroblasts retaining their synthetic (cell proliferation) role rather than differentiating into myofibroblasts (resulting in wound contraction) or disappearing. This results in a profibrotic state and the production of exuberant granulation tissue (EGT), which contributes to wound expansion, delayed contraction and inhibition of epithelialisation. With migrating keratinocytes inhibited, the signalling for apoptosis of fibroblasts is reduced thereby perpetuating the production of further granulation tissue.
Initial management of a chronic wound
Chronic non-healing wounds should be examined with digital exploration, assessing for the presence of foreign material such as bone, wood, metal, grit, suture material, etc. Draining tracts may be present to guide the exploration; however, in some cases, the foreign material may be walled off beyond palpation. Radiography, ultrasonography and even CT or MRI may be useful. In the author’s experience, ultrasound is particularly useful in assessing non-healing wounds as it is highly sensitive in detecting wound tracts, sequestra, suture materials, etc.
Chronic non-healing wounds should be examined with digital exploration, assessing for the presence of foreign material such as bone, wood, metal, grit, suture material, etc
Infection should be suspected if the wound is painful to palpate, malodorous or oedematous, or has discoloured granulation tissue or draining tracts. While obtaining a swab for culture and sensitivity is recommended given the possibility of multi-resistant Staphylococcus aureus, adequate debridement and removal of any foreign material represents the most effective way of reducing wound infection.
Management of exuberant granulation tissue

There are two facets to managing EGT: one is managing the tissue itself and the other is preventing it from reforming. EGT is most effectively removed by excising it when it protrudes above the wound margins (Figure 2).
Preventing recurrence of EGT requires an understanding of why it occurred. Certainly horses are prone to the development of EGT as they have a less intense and more prolonged inflammatory response compared to ponies (Wilmink et al., 2002, 2003). This means they are more likely to develop wound complications such as ongoing infection, which perpetuates the inflammatory phase and therefore the production of EGT (Wilmink et al., 1999). If the presence of infection has been ruled out, a single application of topical corticosteroids or a non-adherent silicone dressing can be effective at reducing the formation of EGT.
Management of distal limb wounds
Distal limb wounds heal more slowly than those on the rest of the body. Wound contraction on limbs is 0.2mm/day compared to 0.8 to 1mm/day (Stashak, 1991). Excessive motion, infection and the development of EGT reduces the rate of epithelialisation and wound contraction. Excessive motion can be ameliorated by keeping the horse on box rest. However, wounds over joints or tendons or in opposition to lines of tension face constant movement and, therefore, contract more slowly, or even stop. While thick distal bandages provide compression to reduce swelling, warmth and protection for the wound, they have minimal ability to restrict motion. A bandage cast is very effective at restricting movement and can often be placed standing; this is especially effective with heel bulb lacerations (Figure 3).




Wounds of the distal limb are more likely to be exposed to contamination with either soil components or faeces. Given horses’ inability to mount an intense inflammatory response, especially in the distal limb, infection is, therefore, more likely. In addition, soil reduces the effectiveness of white blood cells, weakens humoral defences and neutralises antibodies. All of these effects reduce the number of bacteria required to overwhelm the host’s immune system (Rodeheaver et al., 1974). Therefore, in non-healing distal limb wounds, effective debridement alongside systemic, regional or topical antimicrobial therapy, or a combination of these, is usually required. If not performed effectively at the initial presentation, this may need to be performed once the infection has established.
Exposed bone
When bone is devoid of periosteum it is slow to develop granulation tissue due to its poor vascularity, while exposed bone desiccates, which may result in sequestrum formation. Any persistent exudate from a wound overlying bone should prompt radiographic and/or ultrasonographic examination to check for the presence of a sequestrum. If found, prompt removal is essential to expediate wound healing.
Management techniques to consider for non-healing wounds
Bandaging
As stated previously, bandaging has undoubted benefits in managing non-healing wounds, but it has long been associated with EGT formation (Berry and Sullins, 2003). This may be associated with the relative tissue hypoxia which occurs under a bandage (Celeste et al., 2013). Microvascular occlusion of the small capillaries within granulation tissue results in tissue hypoxia which, in turn, causes upregulation of angiogenic and profibroblastic signals (Deschene et al., 2012). In addition, reduced oxygen diffusion results in increased glucose use and lactate accumulation; this too results in angiogenesis and collagen deposition and, subsequently, the formation of EGT (Sørensen et al., 2014). It remains unclear when bandaging becomes detrimental to a wound, but removal of a bandage should be considered in cases of non-healing wounds where another underlying cause is not apparent.
Delayed secondary closure
Delayed secondary closure (after granulation tissue has formed in the wound) is particularly useful for chronic non-healing wounds which have not previously been sutured or have undergone dehiscence after primary closure. The wound bed undergoes en bloc debridement with sharp removal of the superficial tissue of the entire surface of the wound. En bloc debridement is effective at removing bacteria and foreign material, as well as irreversibly damaged tissue. If possible, the wound should be closed at this point, using appropriate tension-relieving techniques (eg undermining the skin edges, mesh expanding incisions and tension-relieving suture patterns). Alternatively, following three to five days of wound management to ensure no further exudate occurs, delayed closure of the wound can be performed. A bandage cast is recommended to reduce motion.
Delayed secondary closure… is particularly useful for chronic non-healing wounds which have not previously been sutured or have undergone dehiscence after primary closure
Skin flaps
A skin flap or pedicle graft is a piece of skin that is moved to cover a defect, but still maintains its blood supply by virtue of its attachment. Skin flaps are less useful on non-healing distal limb wounds as the donor site may become a problematic wound in itself. Narrower flaps are easier to move but are more likely to compromise their blood supply than wider flaps.
A transposition flap is a rectangular pedicle flap which can be rotated up to 180° to cover a defect, while bipedicle advancement flaps are created by making a single longitudinal incision on one side of the wound (Figure 4). The incision is made parallel to the wound edge the same distance from the wound as the width of the defect needing to be closed. As the flap is attached at two sites it has two sources of blood supply ensuring its survival. The flap is completely undermined allowing it to be moved across, thereby closing the original defect. The new defect can then be partially closed following undermining or left to heal by second intention.





Island grafts
If a healthy bed of granulation tissue is present but epithelialisation is failing to proceed, island grafts should be considered. Island grafts are completely separated from the donor site and transferred to a healthy bed of granulation tissue at the recipient site where new vascular connections must be established. The author recommends punch and pinch grafts as the most practical field solution.
If a healthy bed of granulation tissue is present but epithelialisation is failing to proceed, island grafts should be considered
Pinch grafts are usually harvested from the area of neck under the mane. To do this, a small cone of skin is elevated using forceps or a hypodermic needle with a bent point and excised using a scalpel blade. The grafts are implanted into pockets created in the recipient granulation bed using a number 15 scalpel blade at an acute angle 3 to 5 mm apart. A graft survival rate of 50 to 75 percent is expected.
Punch grafts are acquired using a skin biopsy punch (typically 7mm). If a small number are needed, they can be taken directly from the donor site under local anaesthetic. Alternatively, an elliptical section of skin can be harvested (eg from the pectoral region) from which the full thickness plugs are taken. Holes in the recipient granulation bed are made approximately 5mm apart using a smaller skin biopsy punch (typically 5mm) into which the harvested plugs are inserted. The site is then bandaged with a non-adherent dressing until the grafts have taken.









